Molluscum contagiosum
Source :
http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001829/
Source:
http://en.wikipedia.org/wiki/Molluscum_contagiosum
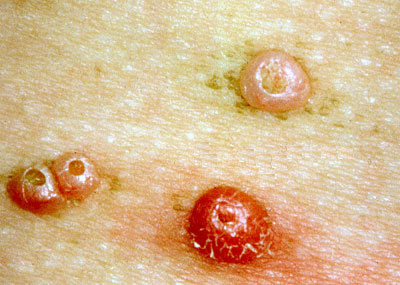
Molluscum contagiosum is a viral skin infection that causes raised, pearl-like papules or nodules on the skin.
Causes, incidence, and risk factors
Molluscum contagiosum is caused by a virus that is a member of the poxvirus family. You can get the infection in a number of different ways.
This is a common infection in children and occurs when a child comes into direct contact with a lesion. It is frequently seen on the face, neck, armpit, arms, and hands but may occur anywhere on the body except the palms and soles.
The virus can spread through contact with contaminated objects, such as towels, clothing, or toys.
The virus also spreads by sexual contact. Early lesions on the genitalia may be mistaken for herpes or warts but, unlike herpes, these lesions are painless.
Persons with a weakened immune system (due to conditions such as AIDS) may have a rapidly worse case of molluscum contagiosum.
Symptoms
Typically, the lesion of molluscum begins as a small, painless papule that may become raised up to a pearly, flesh-colored nodule. The papule often has a dimple in the center. These papules may occur in lines, where the person has scratched. Scratching or other irritation causes the virus to spread in a line or in groups, called crops.
The papules are about 2 - 5 millimeters wide. There is usually no inflammation and subsequently no redness unless you have been digging or scratching at the lesions.
The skin lesion commonly has a central core or plug of white, cheesy or waxy material.
In adults, the lesions are commonly seen on the genitals, abdomen, and inner thigh.
Signs and tests
Diagnosis is based on the appearance of the lesion and can be confirmed by a skin biopsy. The health care provider should examine the lesion to rule out other disorders and to determine other underlying disorders.
Treatment
Individual molluscum lesions may go away on their own and are reported as lasting generally from 6 to 8 weeks,[4] to 2 or 3 months.[5] However via autoinoculation, the disease may propagate and so an outbreak generally lasts longer with mean durations variously reported as 8 months,[4] to about 18 months,[6][7] and with a range of durations from 6 months to 5 years.[5][7]
Treatment is often unnecessary[8] depending on the location and number of lesions, and no single approach has been convincingly shown to be effective. It should also be noted that treatments causing the skin on or near the lesions to rupture may spread the infection further, much the same as scratching does.[9] Nonetheless, treatment may be sought for the following reasons:
Molluscum lesions on an arm.
* Medical issues including:
o Bleeding
o Secondary infections
o Itching and discomfort
o Potential scarring
o Chronic keratoconjunctivitis
* Social reasons
o Cosmetic
o Embarrassment
o Fear of transmission to others
o Social exclusion
Many health professionals recommend treating bumps located in the genital area to prevent them from spreading.[7] The virus lives only in the skin and once the growths are gone, the virus is gone and cannot be spread to others. When treatment has resulted in elimination of all bumps, the infection has been effectively cured and will not reappear unless the patient is reinfected.[10] In practice, it may not be easy to see all of the molluscum contagiosum bumps. Even though they appear to be gone, there may be some that were overlooked. If this is the case, one may develop new bumps by autoinoculation, despite their apparent absence.
Expectations (prognosis)
Molluscum contagiosum lesions may persist from a few months to a few years. These lesions ultimately disappear without scarring, unless there is excessive scratching, which may leave marks.
Individual lesions usually disappear within about 2 - 3 months. Complete disappearance of all lesions generally occurs within about 6 - 18 months. The disorder may persist in immunosuppressed people.
Complications
Persistence, spread, or recurrence of lesions
Secondary bacterial skin infections
Calling your health care provider
Call for an appointment with your health care provider if you have symptoms suggestive of molluscum contagiosum. Also call for an appointment with your health care provider if lesions persist or spread, or if new symptoms appear.
Prevention
Avoid direct contact with the skin lesions. Do not share towels with other people.
Avoiding sex can also prevent molluscum virus and other STDs. You can also avoid STDs by having a monogamous sexual relationship with a partner known to be disease-free.
Male and female condoms cannot fully protect you, as the virus can be on areas not covered by the condom. Nonetheless, condoms should still be used every time the disease status of a sexual partner is unknown. They reduce your chances of getting or spreading STDs. Use them with spermicide with nonoxynol 9.